

The issues surrounding the prevention, diagnosis, and treatment of bovine respiratory disease (BRD) are certainly nothing new to our readers.
BRD is the most commonly diagnosed disease process in cattle, and the most costly, with industry wide economic losses due to BRD estimated at over $1 billion.3
The difficulties surrounding BRD management are in large part due to the wide range of factors that determine disease susceptibility.
These include: 1) animal factors such as age, immune status, and stress; 2) environmental factors such as weather and animal density; and 3) pathogen characteristics including numerous types of both viruses and bacteria.
Traditional dogma assumes the majority of cases are the result of initial viral infections that suppress the calf’s immune system, allowing for bacterial proliferation and subsequent disease.
However, it is clear that bacteria can also be primary pathogens without virus involvement.

Something readers may be less familiar with is the growing concern that strains of bacterial pathogens (both animal and human) are increasingly showing resistance to antibiotics that we have relied heavily on for treating diseases such as BRD in the past.
The discussion of antimicrobial resistance (AMR) is becoming more and more popular among veterinarians, microbiologists, industry leaders, and government officials who are concerned about future ramifications on not only animal health but human health.
Overuse of antibiotics is assumed to play a role in the development of AMR.
The relative impact of antibiotic use in food animals and how this relates to the increased number of AMR bacteria we are seeing on the human side is somewhat controversial (and a much longer discussion for another day), but it is safe to assume that it likely plays at least some role.
The concern over AMR is the driving force behind the implementation of the veterinary feed directive (VFD) in 2017 and the elimination of over-the-counter sales of many popular antibiotics taking effect in June of this year when prescriptions will be required for these drugs moving forward.
Responsible, or judicious, use of antibiotics by producers and veterinarians will be important as we move forward, and being aware of this issue is crucial.
Judicious use of antibiotics in animals can be broadly summarized as using antibiotics only when they are indicated, at the appropriate dose and route of administration, for the appropriate period of time, and choosing the correct class of antibiotic for the given disease process or pathogen.1
Following these principles will eliminate money wasted on needless antibiotic usage, increase the likelihood of a positive treatment outcome, and minimize the likelihood of or need for additional future regulations.
Diagnostic tests for BRD and AMR have improved in the recent past with the development of polymerase chain reaction (PCR) testing availability.
Traditionally, bacteria were grown in a laboratory and diagnosed to the species level based on how the bacteria grew in a number of different media environments.
Then, the bacteria were grown in the presence of a number of antibiotics to determine which antibiotics inhibited growth and therefore might make good treatment options for the particular case.
The advancement of PCR technology has decreased the turnaround time and dramatically increased the sensitivity of bacterial testing compared to culture alone.
That is, we can now have results much quicker and we can detect much smaller amounts of a pathogen since we are amplifying and detecting the DNA itself without relying on the bacteria to grow.
Another benefit is we can determine the quantity of relative pathogens in the sample using many of these newer PCR tests.
This is an important advantage since we can occasionally find BRD-associated bacteria in the respiratory tract of healthy cattle, but knowing there is an exceptionally large amount in a diseased calf lung is a strong indication that the particular bacteria is playing a role in disease.
Culture is still widely used in veterinary diagnostic laboratories and remains the gold standard for identifying and determining the antimicrobial susceptibility of BRD bacterial pathogens.
However, characterization and detection of the genes in BRD-associated bacteria that allow for resistance to two common classes of cattle antibiotics has allowed for even more refined PCR testing.
In 2021, a new PCR test was developed that can detect some of the bacterial genes that confer resistance to macrolide (i.e., Zuprevo®, Draxxin®, Zactran®, Micotil®) and tetracycline (i.e., LA 200) antibiotics.2
This new PCR test dramatically decreases the time needed for antimicrobial susceptibility results since culture is not required.
At the same time, the accuracy of results concerning resistance is comparable to the gold standard method of culture.
This new PCR test for AMR genes to macrolide or tetracycline antibiotics is quantitative and can be performed on either lung tissue from a dead animal or a nasal swab in a live animal.
I believe incorporating the new AMR PCR testing into the management of BRD can be potentially beneficial to beef producers and their veterinarians in two primary ways:
1) Confirming the likelihood of efficacy for antibiotics being used to treat BRD during an outbreak.
Respiratory outbreaks can develop quickly, and prompt treatment is often of critical importance to minimize death losses. Therefore, experience and knowledge of antibiotics usually guides veterinarians to prescribe specific antibiotics in certain situations.
This is true for individual animal treatment protocols or for mass medication of a large group of calves. If a macrolide or tetracycline class of antibiotic is used, the AMR PCR test can be useful to confirm that the bacterial component of the current BRD outbreak does not possess large numbers of antibiotic resistant genes for these drug classes.
Lung tissue from dead calves can be used to test for these genes when assessing a treatment protocol. In the case of mass medicating a group of calves, if a macrolide or tetracycline is chosen, nasal swabs can be obtained from live animals during processing to gauge the likelihood of antibiotic resistance in the specific cohort.
If there are high numbers of resistance genes present in the sample, medicating the group with a different class of antibiotics may be indicated if clinical signs start to suggest a treatment failure.
2) Choosing drugs to be used for metaphylaxis.
Administering antibiotics to all cattle in a specific cohort regardless of their current disease status is referred to as metaphylaxis and this tactic is commonly used to prevent disease, particularly in cattle at higher risk for developing BRD (freshly weaned, multiple ranch source, long-haul, etc.).
As a general rule, macrolide antibiotics tend to provide therapeutic levels of the drug in tissues for longer periods of time compared to other classes of drugs. Therefore, they make good candidates for metaphylaxis and are one of, if not the most common class of drug used for this purpose in feedlot cattle.
If it is anticipated that a macrolide or tetracycline antibiotic will be used for metaphylaxis in an incoming group of cattle, deep nasal swabs can be obtained at the auction market or ranch of origin and submitted for testing before the animals arrive.
In this scenario, the veterinarian and feedlot personnel will have results as to the relative amount of antibiotic resistance genes present in the samples ideally before the cattle arrive, and certainly shortly after arrival in a worst-case scenario.
If there appear to be high levels of macrolide resistance genes in these particular cattle, it may be indicated to choose another antibiotic class for the metaphylaxis.

The AMR PCR test has the potential to be a valuable tool in the management of BRD, but it is not without its own limitations.
The most obvious limitation is that we are currently only able to test for resistance genes to two antibiotic classes. While these two classes represent a large percentage of antibiotics used in cattle, there are other important classes which will continue to require traditional culture methods for AMR susceptibility testing such as the fluoroquinolones (i.e., Baytril®), cephalosporins (i.e., Excede®), and florfenicols (i.e., Nuflor®) among others.
Another limitation to the AMR PCR test is that we do not know precisely what level of antibiotic resistance genes in a given sample is significant in terms of predicting treatment failure in the field. It is safe to assume that the higher the amount of resistant genes in a sample, the higher likelihood there is for clinical resistance, but a precise level where there is cause for concern is currently unknown.
Therefore, to most efficiently use the assay in its current form, it would be worthwhile to sample a random subset of calves to get an overall gauge on the magnitude of resistant genes present among the group to help guide drug choices.
Finally, the AMR PCR does not detect all genes asso ciated with macrolide or tetracycline resistance. Therefore, it is recommended to be used in conjunction with culture-based methods since there are other genes that may be conferring resistance in a given strain.
That being said, detecting high levels of resistance genes via the AMR PCR in combination with pathogen detection can be useful clinically.
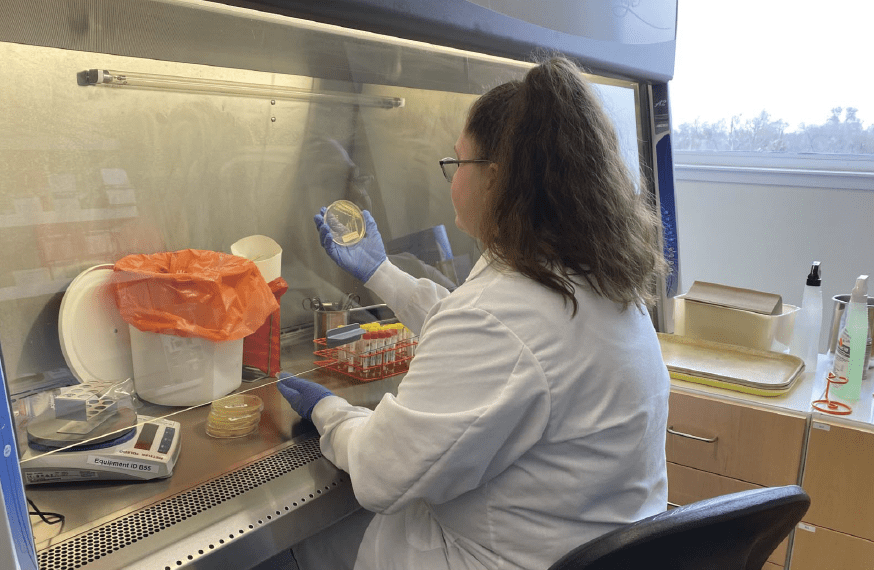
The AMR PCR test is currently offered at the Nebraska Veterinary Diagnostic Center (NVDC). It is likely other diagnostic laboratories will offer this service in the future.
At the NVDC, the test can be ordered alone or along with multiplex PCR testing for the most common viral and bacterial pathogens and culture as a “complete BRD PCR test” for a reduced cost compared to ordering each test individually. The turnaround time for results is 48-72 hours under normal conditions and the test can be performed on lung tissue, swabs, or previously isolated strains of bacteria.
References
1. Judicious therapeutic use of antimicrobials: American Veterinary Medical Association, 2023: https://www.avma.org/resources-tools/avma-policies/judicious-therapeutic-use-antimicrobials.
2. Dutta E, et al. Development of a Multiplex Real-Time PCR Assay for Predicting Macrolide and Tetracycline Resistance Associated with Bacterial Pathogens of Bovine Respiratory Disease. Pathogens 2021;10.
3. Griffin D, et al. Bacterial Pathogens of the Bovine Respiratory Disease Complex. Veterinary Clinics of North America: Food Animal Practice 2010;26: 381-394.
 Dr. Matt Hille is an assistant professor at the University of Nebraska-Lincoln where he serves as a diagnostic pathologist and extension veterinarian at the Nebraska Veterinary Diagnostic Center. He was a cow/calf and feedlot veterinarian in South Dakota for a number of years prior to pursuing a career as a diagnostician. His diagnostic and research interests are focused on infectious diseases of food animals with a particular interest in beef cattle. He is a graduate of Iowa State University (DVM), the University of Wyoming (M.S.) and the University of Nebraska (Ph.D.). Matt and his wife, Katie, live in Lincoln, Nebraska, with their three children where they attend as many Husker football games as possible.
Dr. Matt Hille is an assistant professor at the University of Nebraska-Lincoln where he serves as a diagnostic pathologist and extension veterinarian at the Nebraska Veterinary Diagnostic Center. He was a cow/calf and feedlot veterinarian in South Dakota for a number of years prior to pursuing a career as a diagnostician. His diagnostic and research interests are focused on infectious diseases of food animals with a particular interest in beef cattle. He is a graduate of Iowa State University (DVM), the University of Wyoming (M.S.) and the University of Nebraska (Ph.D.). Matt and his wife, Katie, live in Lincoln, Nebraska, with their three children where they attend as many Husker football games as possible.
Get all Doc Talk episodes straight to your email inbox!